
The Rising Burden of Childhood Obesity: Prevention Should Start in Primary School
Childhood obesity is increasing and is a significant global public health challenge. Worldwide, about 41 million children under the age of 5 years have overweight, and 340 million children and adolescents aged 5 to 19 years live with obesity1. The onset of obesity can start from an early age, and so a preventative multidimensional approach focused on modifiable lifestyle factors is needed early in life.
Nutrition and physical activity are well recognised as lifestyle factors that play a key role in the prevention of obesity, and more recently research has highlighted the importance of sleep2,3.
A recent research paper written by Prof Malgorzata Gabriela Wasniewska, Dr Giorgia Pepe, Dr Domenico Corica, Prof Tommaso Aversa, Dr Debora Porri and Dr Letteria Morabito from Obelisk partner the University of Messina, addresses the increasing prevalence of childhood obesity and emphasises the need for early prevention through lifestyle interventions.
The study, part of the regional Italian project "EpPOI: Education to Prevent Childhood Obesity", focuses on adherence to the Mediterranean diet, physical activity, and sleep habits among preschool children to prevent childhood obesity early. This article explores the key findings of the research and examines how these lifestyle factors contribute to children's overall health and well-being.
What Did the Study Involve?
The study gathered data from parents of 4-5-year-old children. A total of 95 mothers completed questionnaires, with the aim of investigating the relationship between lifestyle habits and health outcomes through parental perception. The questionnaires asked about the child’s diet quality, using the Mediterranean Diet Quality Index for children and adolescents (Kid-Med), parents’ perception of how physically active their child is, sleep hygiene, including quantity of sleep and use of electronic devices.
Key Findings from the Study
Key findings include:
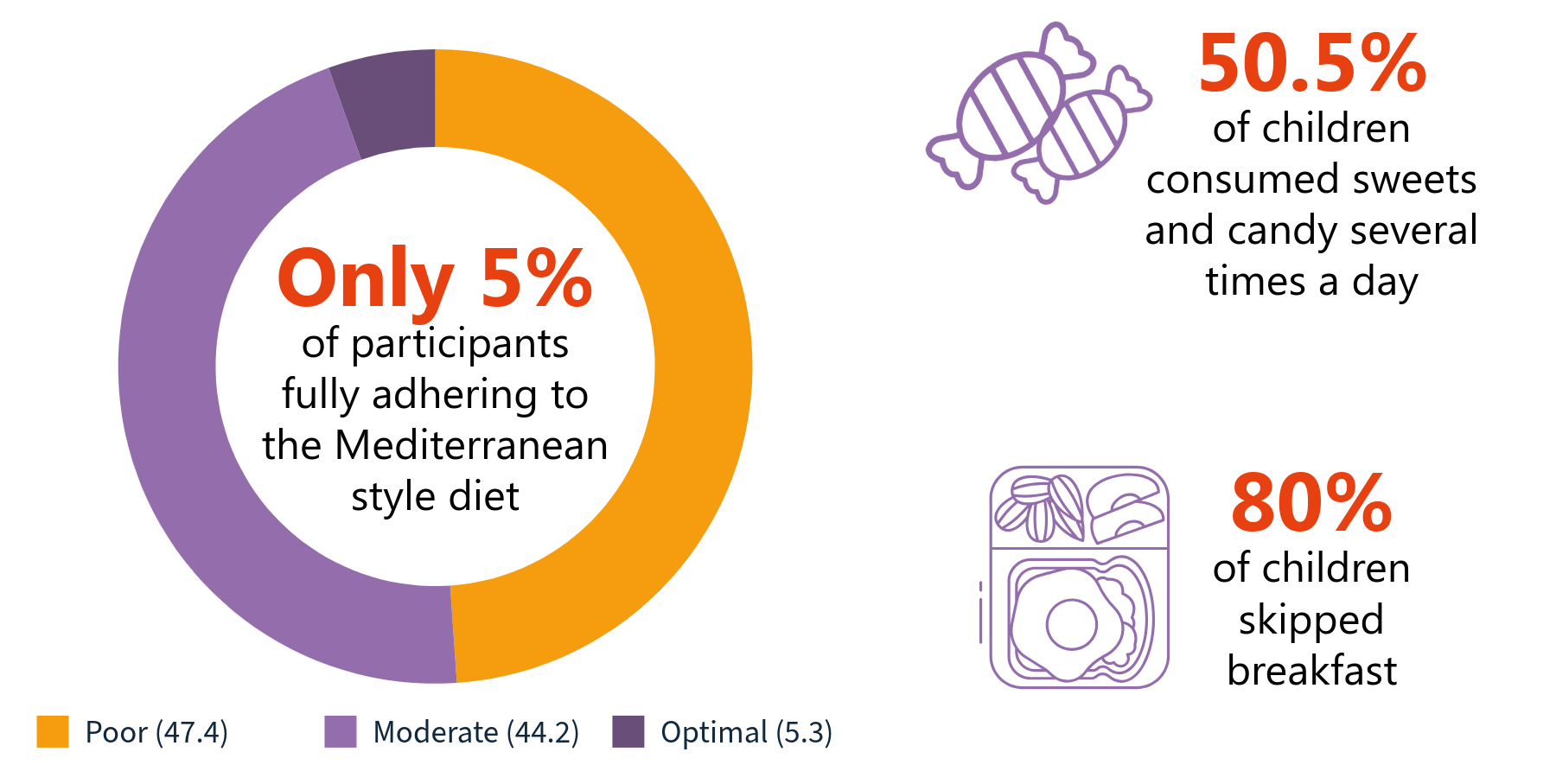
- Low adherence to the Mediterranean diet: Only 5.3% of children achieved optimal adherence to the Mediterranean diet, with 47.4% showing poor adherence. High consumption of sweets (50.5%) and skipping breakfast (80%) were common.
- Parental perception and physical activity: Parents' perception of their child's physical activity was positively correlated with better adherence to the Mediterranean diet, including higher fruit, vegetable, and fish consumption, and lower intake of sweets.
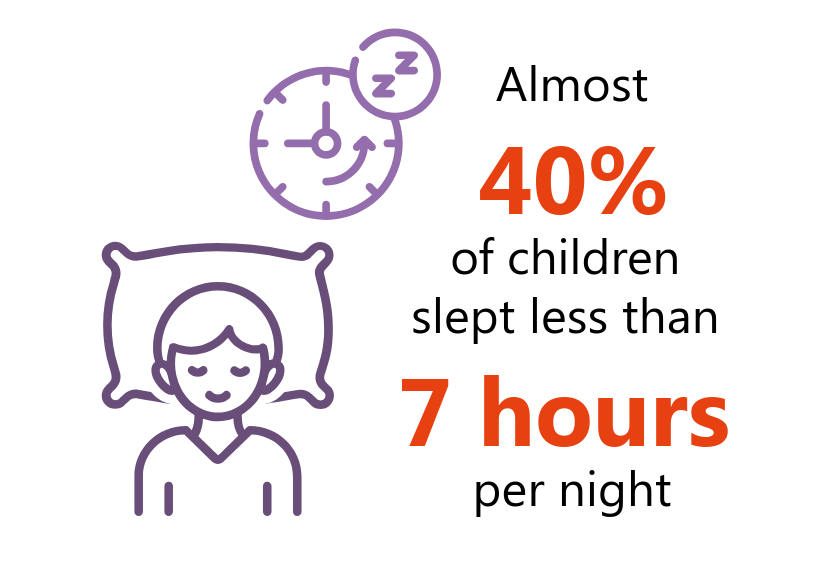
- Sleep and screen time: While 62.8% of children slept more than seven hours a night, 37.2% slept less. Increased screen time and reduced physical activity during the COVID-19 pandemic were linked to unhealthy habits and weight gain.
The study provides valuable insights into preschool children's lifestyle habits, including diet, physical activity, and sleep. Each of these areas plays a crucial role in shaping children's long-term health. In the following sections, we begin by outlining the key findings from the study before exploring each behaviour to understand its impact on healthy growth and the prevention of childhood obesity.
The Mediterranean Diet
Only 5% of the participants in the study were adequately adhering to a Mediterranean-style diet. The Mediterranean diet positively impacts childhood obesity by promoting a balanced intake of nutrient-rich foods that help prevent weight gain and support overall health.
Beyond the findings of this study, the Mediterranean diet has been widely recognised for its health benefits:
- Nutritional benefits: The Mediterranean diet emphasises fruits, vegetables, whole grains, legumes, fish, olive oil, and nuts, while limiting red meat and sweets. This nutrient-dense profile is rich in bioactive compounds with anti-inflammatory and antioxidant properties. Many of these foods are inversely associated with obesity.
- Lower body mass index (BMI): Studies show that greater adherence to the Mediterranean diet is associated with a lower BMI in children and a decreased prevalence of obesity.
- Parental influence: Children are more likely to adopt the Mediterranean diet when parents model healthy eating behaviours, reinforcing its benefits in the family environment. Habits established in the family home as children often follow through into adulthood, so having this style of diet from a young age at home and in school can create lifelong healthy habits.
- Preventive role: The Mediterranean diet helps counter the growing trend of eating more processed foods and sugary drinks, which are spreading worldwide and linked to childhood obesity.
Overall, the Mediterranean-style diet provides a sustainable and effective dietary framework for reducing childhood obesity and promoting long-term health. Of course, there can be social and financial barriers to families being able to effectively adhere to this style of eating that requires wider political change to increase the availability of this diet to more children and families.
Physical Activity
The study found parents' perception of their child's physical activity was positively correlated with better adherence to the Mediterranean diet, including higher fruit, vegetable, and fish consumption, and lower intake of sweets. Conversely, if parents perceived their child’s physical activity as low, the child was more likely to consume sweets several times a day (50.5% of children consumed sweets and candy several times every day). This finding suggests that lifestyle behaviours can be linked- the more or less you do of one can lead to more or less of other modifiable lifestyle behaviours.

World Health Organization Guidelines on Physical Activity
Physical activity is an important lifestyle factor to focus on in early childhood as:
- Physical activity is a protective factor against obesity. Guidelines recommend that school-aged children engage with at least 60 minutes of moderate to vigorous activity a day4, and children under 5 require 180minutes of physical activity a day5. Those who adhere to this are less likely to become overweight or obese.
- Excessive screen time (TV, tablets, phones, computers) is strongly associated with higher BMI in children. Longer screen use often replaces physical activity and is linked to mindless snacking, exposure to junk food advertising, and poor sleep, all risk factors for obesity.
- Physical activity and screen habits formed in early childhood tend to persist into adolescence and adulthood. Intervening in primary school years to promote active play, reduce screen exposure, and build structured daily routines can have long-term benefits for preventing obesity.
Sleep
This research found nearly 40% of children slept less than 7 hours a night, which is well below the recommended 10-12hours for school-age children.
This finding is of importance as children who sleep less than the recommended amounts have been seen to have higher BMIs and are more prone to weight gain over time. This can be for several reasons:
- Sleep deprivation can alter appetite regulation by affecting hormones involved in appetite regulation, leading to increased hunger and energy intake. Lack of sleep has been seen to make foods more rewarding and may influence dietary choices6. Energy intake and perceived appeal of sweet foods have also been found to increase in sleep-deprived children7.
- Evidence has shown a link between lack of sleep and metabolic dysregulation in children, which can increase the risk of obesity, meaning sleep may be an overlooked component of obesity prevention2. Sleep duration is thought to influence metabolic health by interacting with the circadian rhythm8, the internal biological clock that regulates metabolism. Insufficient sleep can disrupt this biological clock and interfere with the function of related cells, potentially leading to metabolic imbalances. This disruption may impair glucose metabolism, insulin sensitivity and over time increase the risk of metabolic disorders and obesity.
- Lack of sleep can also lead to behavioural and lifestyle effects. Tired children are:
-
- Less likely to engage in physical activity.
- More likely to spend time in sedentary behaviours, like screen time.
- More prone to emotional eating or late-night snacking.
Recommendations from the Study
The study provides some recommendations for effective childhood obesity prevention. The researchers urged that interventions should begin early, particularly in primary school, where healthy behaviours can be taught and reinforced during critical developmental years. The recommendations include:

Looking Ahead: The Need for Future Research
This study has given an interesting insight into the relationship between lifestyle habits and health outcomes through parental perception in this sample group in Italy. More research like this would be useful to see the current picture in other communities. The researchers also suggest future research should further explore socio-cultural factors, such as caregiver attitudes and community support systems, in enhancing adherence to healthy dietary patterns such as the Mediterranean diet.
How Obelisk is Supporting the Study Recommendations
The Obelisk project recognises that to address the growing challenge of childhood obesity, we need a multifaceted approach that integrates a family-centred approach to integrating nutrition education, access to food and physical activity promotion. In our Empowering Adolescents with Obesity to Unite for a Better Society - ADOBESIF Trial- we are specifically aiming to engage with families with low incomes, and researching areas such as socio-economic status and parental attitudes, whilst offering nutrition education physical education sessions, via hip-hop dance classes. One further benefit, for one of the intervention groups, is a weekly supply of food parcels with fast, healthy recipes tailored to the family’s preferences and habits. We aim to improve our understanding of the broader societal and individual factors influencing dietary preferences and food intake, and the links between nutrition and exercise.
Paper
Porri, D., Wasniewska, M., Luppino, G., Morabito, L. A., La Rosa, E., Pepe, G., Corica D., Valenzise M., Messina M.F., Zirilli G., et al. The Rising Burden of Childhood Obesity: Prevention Should Start in Primary School. Nutrients (2025)., 17(4), 650.
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults.Lancet2017, 390, 2627–2642.
- Porri, D., Luppino, G., Aversa, T., Corica, D., Valenzise, M., Messina, M. F., ... & Wasniewska, M. G. (2024). Preventing and treating childhood obesity by sleeping better: a systematic review. Frontiers in Endocrinology, 15, 1426021.
- Gale, E.L.; James Williams, A.; Cecil, J.E. The relationship between multiple sleep dimensions and obesity in adolescents: A systematic review. Med. Rev.2024, 73, 101875.
- WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO
- World Health Organization. (2019). Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. World Health Organization. https://iris.who.int/handle/10665/311664. License: CC BY-NC-SA 3.0 IGO
- Soltanieh S, Solgi S, Ansari M, Santos HO, Abbasi B. Effect of sleep duration on dietary intake, desire to eat, measures of food intake and metabolic hormones: A systematic review of clinical trials. Clin Nutr (2021) 45:55–65. doi: 10.1016/j.clnesp.2021.07.029
- Simon SL, Field J, Miller LE, DiFrancesco M, Beebe DW. Sweet/dessert foods are more appealing to adolescents after sleep restriction. PLoS One. (2015). 10:e0115434. doi: 10.1371/journal.pone.0115434
- Lyu J, Lee K, Jung S, Park YJ. Associations of meal timing and sleep duration with incidence of obesity: a prospective cohort study. J nutrition Health aging. (2024)28:100220. doi: 1016/j.jnha.2024.100220